ARTICLE AD BOX
It was September 2017 at a teaching hospital in Nigeria’s southern state of Bayelsa. An 11-year-old boy came into the clinic with a fever, rash and lesions on his body.
Infectious disease scientist and Chief Medical Director Dimie Ogoina examined him. At first, doctors thought it could be chickenpox, but after hearing the boy had previously had the illness, they suspected it must be something more serious.
Upon further examination, Ogoina concluded that it was likely monkeypox, a highly infectious disease that causes a skin rash, mucosal lesions and other symptoms the boy was experiencing.
It was a stunning finding. The last case of monkeypox – now called mpox – detected in Nigeria was nearly 40 years earlier. And even then, there were only two cases ever recorded. The country was not prepared for it.
At that point, Ogoina couldn’t be certain of the diagnosis, though. He first had to notify the Nigeria Centre for Disease Control and Prevention, which needed to take a sample and then send it to the Institut Pasteur in Dakar, Senegal, for testing. The process took days, but when the results came in, it was as Ogoina had suspected.
As alarm bells rang through Nigeria, more suspected cases started to stream into his hospital. Every one had to be tested and confirmed from Dakar.
Fear, stigma and speculation grew and were palpable inside the hospital. They were aided by fake theories spreading in the media about “another Ebola” – the haemorrhagic viral disease that hit the country just three years before.
The 11-year-old, on returning home healthy again, was taunted by neighbours as “monkey boy”. Other misconceptions also emerged: One man who’d been traced from an infected female sexual partner refused to report to a hospital, insisting his sickness was a “spiritual attack” and would be cured as such.
Some patients could not bear the fear and waiting.
“We lost [a] patient to suicide – she died even before the results came out,” said Ogoina, who is still on the front lines of detecting and treating mpox cases, seven years since he sounded that first alarm.
“We had challenges telling the family, and we had to use some diplomacy to resolve that problem. Sometimes outbreaks are not just medical challenges. They are social challenges as well,” he told Al Jazeera.
 A health official leaves a room in which a probable case of mpox is being treated in Tshopo, the Democratic Republic of the Congo, during the 2022 outbreak [File: Arlette Bashizi/Reuters]
A health official leaves a room in which a probable case of mpox is being treated in Tshopo, the Democratic Republic of the Congo, during the 2022 outbreak [File: Arlette Bashizi/Reuters]Last month, the World Health Organization (WHO) declared mpox a public health emergency of international concern (PHEIC) – its highest alert level. Ogoina sits on the global expert panel that prompted the WHO to issue the declaration.
It’s the second time in two years that the mpox virus is on the move. This time, a new, faster-spreading variant is flitting across continents and sparking concerns of another serious epidemic.
Cases in the new outbreak have been recorded in about 15 countries in East and West Africa, Asia and Europe. This follows dozens of countries reporting cases in a previous outbreak that started in 2022.
The origins and history of mpox go back decades. It was first discovered in Denmark in 1958 in monkeys that were kept for research. The first case in humans was detected in 1978 in a nine-month-old baby in the DRC.
After that, the disease steadily emerged in West and Central Africa, spreading in two distinct strains, clade 1 and clade 2. Since 2005, cases have been reported in the DRC, usually flaring in remote areas and then petering out. But since 2017, when mpox re-emerged in Nigeria, it has spread among people and travellers in the region.
New medical findings
As the 2017 Nigerian outbreak grew, Ogoina’s hospital was forced to improvise.
The country did not have the ability to test for the disease. At the same time, there were also no isolation centres, so his team hastily turned one ward into a cordoned-off area for both male and female patients. Soon, one of the doctors caught the disease.
Added to the physical challenges and limitations, Ogoina had other headaches as well.
Unlike past outbreaks of the disease that were recorded in the DRC, patients were presenting with rashes and lesions on their genitals – areas that most people find sensitive to report in a hospital. Some were instead visiting small medicine kiosks that dot Nigeria so they could treat themselves, meaning more cases were likely being transmitted under the radar.
It is now known that mpox spreads by close contact and skin-to-skin touch with someone who has the disease – including through kissing and sex. But when the first cases were discovered in the 1970s, mpox was thought to be contracted from animals and believed to be more dangerous and common in children.
 People wait at an mpox treatment site in Munigi, DRC, in August 2024 [Moses Sawasawa/AP]
People wait at an mpox treatment site in Munigi, DRC, in August 2024 [Moses Sawasawa/AP]In 2017, Ogoina noticed that a different population appeared to be most affected.
“I was like, ‘Why are we having young men between 30 and 35?’ I’ve read the literature, and it’s most common among children. … And why are they having genital ulcers?” he wondered.
Many of the patients were also HIV-positive. Ogoina suspected sexual transmission, but this had never been documented before. “I wanted to explore that. I remember even developing a questionnaire to get their sexual history, but people thought I was mad. But I said, ‘This is a new type of mpox.’”
Ogoina put his findings in research papers but was met with harsh pushback. One review of his work read: “It is quite reckless to speculate [about] possible sexual transmission as no epidemiological data are available in the literature.”
It was during the 2022-2023 global outbreak that scientists found evidence that some variants of mpox were indeed sexually transmittable. Doctors found most cases at that time did not present in children as in the past, but largely in groups of men who have sex with men or heterosexuals who engage with multiple partners. The disease was also spreading from person to person for a sustained period rather than from animals to humans. And the first cluster of cases was found in London and traced back to a British national with a travel history to Nigeria, where it was believed to have been circulating for years.
Although science would eventually confirm Ogoina’s findings, in 2017 the criticisms he heard were “discouraging” and made him less certain about putting his theories out into the world, he said.
However, the scientist took the rejections gracefully.
“If I was on the other side, I would also have had doubts, and that’s the beauty of science,” Ogoina said. A doctor from a small hospital in the smallest state in Nigeria with no access to labs, isolation wards and with fewer than 100 patients pushing a new theory on mpox? There of course was going to be someone who challenged those findings.
Nigeria has gone on to build several laboratories although Ogoina worries maintaining them might be an issue.
 A man reads a newspaper on a Lagos street during an outbreak of Ebola in West Africa in 2014 [File: Sunday Alamba/AP]
A man reads a newspaper on a Lagos street during an outbreak of Ebola in West Africa in 2014 [File: Sunday Alamba/AP]Deadly diseases in difficult conditions
The mpox virus and the way it operated was largely unknown to many outside the endemic areas until it went global in 2022 and affected more than 100,000 people in 120 countries, most of which had never dealt with the disease before.
Now, after the WHO’s alarm, there are particular fears about the spread of a new, possibly more dangerous variant of mpox that emerged in September last year, clade 1b – which is separate from the milder clade 2, which caused the 2022 global outbreak.
The WHO has pointedly said, “This is not another COVID-19,” but its PHEIC alarm usually is a prelude to significant outbreaks, like the Ebola and Zika epidemics.
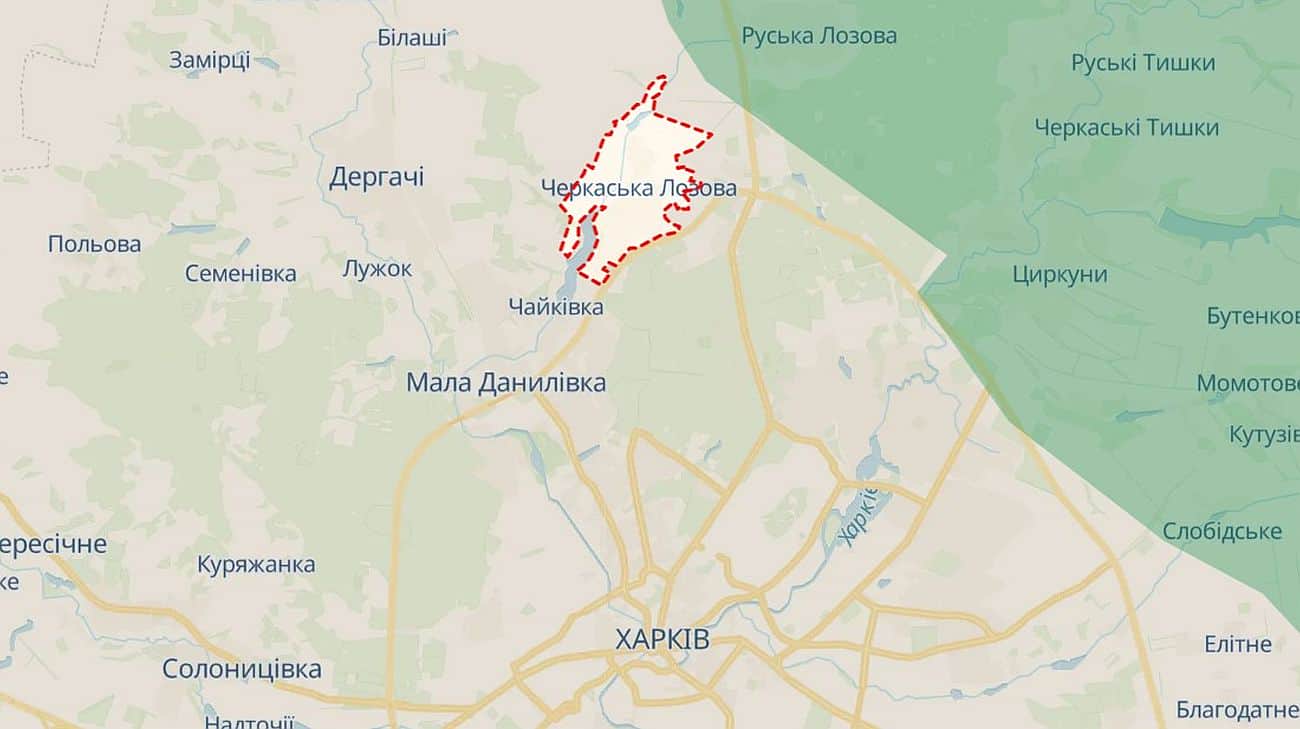
The DRC reported the first case in the outbreak two years ago. Mpox is endemic in the country, but the new scourge comes at a hard time.
In Goma, near the epicentre of the virus in the country’s east, health workers are having to treat patients covered in itchy lumps and painful lesions even as war closes in: Just northeast of the city, the M23 armed group is advancing, looking to take Goma in its long battle with the Congolese government.
In addition, hospitals in Goma are struggling with low laboratory capacity to test suspected mpox cases. Diagnostic kits being deployed there are not doing a thorough job, making it harder to track cases, health workers said.
However, it’s the lack of a single vaccine dose in the country more than 24 months after the outbreak started that’s striking for many. Western countries deployed widespread vaccinations to bring the 2022 outbreak under control within a year. The DRC and other African countries affected in this outbreak, though, have not had the same luxury. Africa does not produce the vaccines. The only two mpox vaccine producers are in Germany and Japan, and the shots are expensive.
Hopes that the DRC had of getting a shipment from Japan last week were dashed due to an administrative delay. Germany has promised to send 100,000 doses, but it’s unclear when those will materialise. Nigeria, however, did receive the first donation of 10,000 doses from the United States.
For Didier Mukeba Tshilala, poor vaccine coverage in the developing world leads to preventable epidemics. The situation is reminiscent of the COVID-19 pandemic when African countries had to wait for vaccines at the same time countries like the US were already administering boosters.
“Africa produces less than 2 percent of the vaccines it needs to protect its population against diseases and epidemics,” said Tshilala, a DRC native who manages East and West Africa operations for the medical charity Doctors Without Borders, also known by its French acronym MSF. African countries are already stretched because they have low health budgets as most prioritise security needs amid several conflicts, he said – like in eastern DRC.
Tshilala was also at the front lines when Ebola and then COVID-19 racked the DRC. But the country is not alone regarding poor healthcare access, he said. Health workers in other parts of Africa, in Latin America and elsewhere have to trace and treat deadly diseases in difficult conditions.
Meanwhile, Western countries are often passive about diseases endemic in these places and spring into action when they become a threat to them, he added.
“As long as this reality persists, we should unfortunately expect recurrent epidemics in Africa. Given the strong interconnection of the world, no country is safe.”
Niche pathogens, new threats
Beyond the known and current threats, scientists are also hard at work detecting what may be next on the horizon.
Daniel Romero-Alvarez has always found “weird pathogens” more interesting, he said, because “everyone else is studying dengue and malaria”.
The Ecuadorian epidemiologist has published paper after paper on some of the most obscure pathogens: the Trematode flatworm or Leishmania parasites.
That fascination with niche pathogens led him to a worrying discovery in 2016: Deforestation was fuelling the spread of a little known but rapidly spreading virus in South American countries.
The scientist with the Universidad Internacional SEK in Quito noted in studies he co-authored in 2016 and 2023 that vegetation decline appeared to correspond to locations reporting more cases of Oropouche, a disease that is speedily being transmitted across countries of the Amazon and that scientists said presents with a mild fever but also causes brain defects. Experts are still researching whether the disease can be transmitted from mother to child in utero amid reports of microcephaly and miscarriages in infected women.
 Smoke rises from fires in the Chico Mendes Extractive Reserve in Xapuri, Acre state, Brazil. Deforestation in the Amazon poses a threat to communities and health [File: Gleilson Miranda/AP]
Smoke rises from fires in the Chico Mendes Extractive Reserve in Xapuri, Acre state, Brazil. Deforestation in the Amazon poses a threat to communities and health [File: Gleilson Miranda/AP]Brazil is the epicentre of an outbreak triggered in late 2023 with more than 7,000 cases reported this year, a surge from about 800 cases in 2023. Bolivia, Cuba, Peru and Colombia have also reported scores of cases. The disease is, so far, rarely fatal. In July, two women in Brazil’s Bahia state became the first casualties. Nineteen cases have been reported in Europe, and 21 in the US – all in travellers from affected countries.
Oropouche is believed to be hosted by sloths, primates, rodents and possibly birds. Humans get sick when they’re bitten by tiny infected flies.
“The virus is transmitted through the bite of a midge, and a midge loves alternate ecosystems like plantations of cocoa and banana,” Romero-Alvarez said. “So it makes sense that if you take out trees from a particular region and replace them with plantations, you’re going to have an explosion of midges.”
First documented in the Caribbean nation of Trinidad and Tobago in 1955 and named after a community there, the disease used to be concentrated in a few countries of the Amazon and Brazil’s Amazon regions but has spread farther outside that range in this outbreak.
Rapid deforestation in the rainforest – the world’s most important ecosystem for storing carbon and combating climate change – has been ongoing for decades. Massive swaths of jungle are giving way to farms and oil drilling sites. Habitat loss in Brazil, which is home to nearly 60 percent of the Amazon, escalated under former President Jair Bolsonaro but has since been halved. In other countries, though, particularly Bolivia, deforestation is surging. Some experts predicted that the Amazon will lose an area the size of the United Kingdom from 2021 to 2025.
Satellite images that Romero-Alvarez and his team analysed showed possible correlations between reduced vegetation and higher reported cases of Oropouche, but the scientist pointed out that establishing direct causal links is more difficult.
Churning out research in a region where governments pay little attention is hard, Romero-Alvarez said. Despite the available evidence, Amazon countries are struggling to end deforestation. At a summit in 2023, Brazil’s current president, Luiz Inacio Lula da Silva, failed to rally the eight Amazon countries to agree to zero deforestation by 2030. One of the harder nuts to crack was Bolivia, which is investing heavily in agriculture. Until this outbreak, the country had never reported a case of Oropouche.
That attitude could prove dire in a region that’s just emerging from the Zika and Chikungunya epidemics and that’s right now battling dengue, Romero-Alvarez said. In his home country of Ecuador, the healthcare system is already burdened on a normal day, and Oropouche cases will only add on to that.
Still, the researcher rarely expects governments to act on data. “I am a cynic about all this stuff,” he said. “It’s like that meme where something really bad is happening around you and you just continue what you’re doing calmly. Governments never take science seriously. You can see that with climate change and with the COVID-19 pandemic. It’s super disappointing.”
It’s hard enough to do the research itself, he pointed out. Some science journals require thousands of dollars in submission fees from researchers like him, for example, and governments are often not cooperative in releasing crucial information needed for his research.
When the frustrations mount, Romero-Alvarez turns to creative outlets. He sings, plays the piano and takes stunning, close-up, glossy photographs of the parasites that intrigue him, like mosquitoes. His singular focus is on his work and his side passions, he said.
“I no longer worry about governments using science. I am worried about the science I do being really good.”
 4 months ago
87
4 months ago
87







 English (US)
English (US)